Abstract
Background. Hospital course of patients with hematologic malignancies associated with multiple complications, such as venous thromboembolism (VTE) which significantly affects morbidity and mortality. Compared to the general population patients with hematologic malignancies carry series of risk factors of VTE. Goals of this study were to describe demographic characteristics as well as define the risk factors of VTE in hospitalized patients with hematologic malignancies. Our study was focused on acute lymphocytic leukemia (ALL), chronic lymphocytic leukemia (CLL), acute myeloid leukemia (AML), chronic myeloid leukemia (CML), Non-Hodgkin's lymphoma (NHL), Hodgkin's Disease (HD), multiple myeloma (MM).
Methods. Cohort selection. The Nationwide Inpatient Sample (NIS) database from the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality (AHRQ) for the years 2011 to 2015 was queried for the analysis. We used International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and corresponding ICD-10-CM codes (for the period of 0ctober 1 - December 31, 2015) in order to identify patients with hematologic malignancies as a primary diagnosis for the hospitalization, and VTE as secondary diagnosis of the hospitalization. In order to determine comorbidities in selected population we used Clinical Classifications Software (CCS) in conjunction with ICD-9-CM codes. Statistical Analysis. Complex weights were used throughout all calculations, enabling appropriate national projections. Percentages in all tables and figures reflect national estimates. Chi-squared and independent t-tests were used for univariate analysis where appropriate. We performed logistic regression analyses to examine the association between risk factor and VTE. In our study p-value <0.05 was considered statistically significant. Data were analyzed using SAS v9.4 (SAS Institute, Cary, NC).
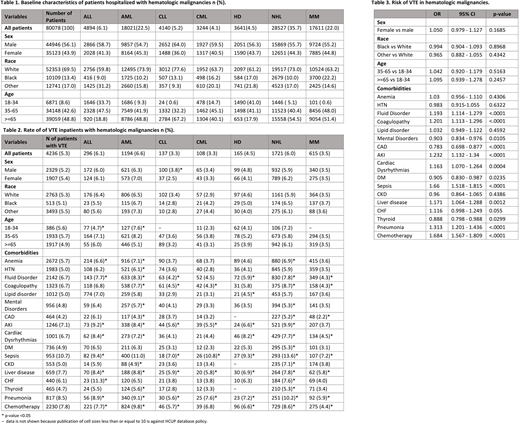
Results. A total of 80,078 patients with hematologic malignancies were hospitalized from 2011 to 2015. Males represented 56.1% of the population, majority of the patients were white (69.5%), greater part of the patients were older than 35 years of age (35-65 42.6%, >65 48.8%) (Table 1). Main comorbidities during hospitalization were anemia (58.1%), followed by hypertension (49.1%), fluid disorders (40.1%) and coagulopathies (24.5%) (data not shown). Rate of VTE in all patients was 5.3% and was evenly distributed among genders and races. Rate of VTE was highest in patients with AML (6.6%) followed by ALL (6.1%), and NHL (6.0%), and lowest in patients with MM (3.49%) followed by CLL (3.31%), and CML (3.31%) (Table 2). The highest risk of VTE among patients with hematologic malignancies were in patients receiving chemotherapy (OR=1.684 95% CI=1.567-1.809) followed by infections such as pneumonia (OR 1.313 95% CI 1.201-1.436) and sepsis (OR=1.66 95% CI=1.524-1.621). Other comorbidities such as congestive heart failure, liver disease, coagulation disorders and acute renal failure were associated with significantly higher risk of VTE with OR varying from 1.1 to 1.2. (Table 3)
Conclusions. In this retrospective large US inpatient database analysis, we found that average rates of VTE in patients with hematologic malignancies was 5.3% and was highest in patients with AML. Patients receiving chemotherapy had highest risk of developing VTE during hospitalization followed by patients with infections such as sepsis and pneumonia. Higher rates of VTE in patients receiving chemotherapy and patients with sepsis was previously described, however our findings indicate that rate of VTE remain high in these population. Findings of our study can be used for development of the appropriate antithrombotic prophylactic strategies in hospitalized patients with hematologic malignancies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal